Featured
Tags
Share
- Home / Blog / Health Professions / COVID-19 and Race - What Do We Know So Far?
COVID-19 and Race - What Do We Know So Far?
COVID-19 cases have surged to a record breaking 199,988 new cases per day (as of December 2, 2020.) With more than 274,000 COVID-19-related deaths in the United States thus far, it is important to start thinking about how this virus affects different populations in our country.
According to the CDC, race and ethnicity are significant risk factors for underlying conditions that contribute to higher COVID-19 infection and death rates. Some of the conditions that impact risk the most include socio-economic status (poverty), access to health care (poverty), and increased exposure to the virus due to occupation (essential and frontline workers, critical infrastructure workers).
What Do We Know About COVID-19 and Race?
So far, we know there is a higher COVID-19 infection and death rate among minority communities. The CDC suggests African Americans and Hispanic Americans are more likely to encounter COVID-19 or have higher risk factors that predispose them to direct contact with the virus. Based on this information, one might conclude that COVID-19 is impacting Black and Brown communities at disproportionate rates, underlying decades of discrimination rooted in structural racism and healthcare inequity.
“When America Catches a Cold, the Black Community Catches Pneumonia”
According to Dr. Gil Singletary, Chamberlain University’s senior director of the College of Health Professions, the above is an adage of the Black community.
"I can remember my grandfather saying this to me as a kid,” said Dr. Singletary, PhD, JD, MBA, MSW, LCSW. “Granted, at the time I didn’t really know the meaning of what he was saying. Now, I think the message is clear. In Chicago, African Americans make up only 30% of the population, but account for 60% of COVID-19 deaths. Similar trends exist in Milwaukee, Detroit, New Orleans, and other areas with dense populations of African Americans.”
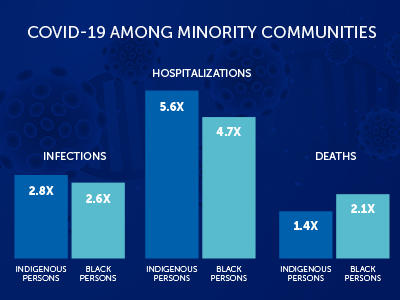
Statistics from the CDC show how much higher the COVID-19 infection, hospitalizations and death rates amongst Black and Indigenous people, as compared to the white population.
There are also striking infection increases in the Hispanic community, who are 2.8x more likely to become infected and 4.6x more likely to be hospitalized. The COVID-19 mortality rate is considerably lower for the Hispanic community, as compared to Indigenous and Black communities.
Based on these statistics alone, it is easy to draw a basic correlation between COVID-19 and race. Clearly conditions that impact marginalized communities (in general) also impact infection and mortality rates.
Race and Comorbidities for COVID-19
Key factors that contribute to higher COVID-19 infection and mortality rates are the presence of underlying comorbidities - such as asthma, hypertension, diabetes, being overweight and being over 65 years of age.
Research shows that Black and Brown people are between 39.5% and 45.2% more likely to have hypertension (variable based on sex). We also know that Black and Brown people are 77% more likely to have diabetes due to comorbidities that are related to biology, diet, socioeconomic situations and access to healthcare.
Dr. Singletary says, “The first social determinant of health is a lack of access to quality medical care. The second is the persistent wealth gap that exists between communities of color and other communities. [Because of a] lack of access to quality health care, many individuals living in Black and Brown communities use emergency rooms like many of us use our primary physician. For many of these individuals, it's their only means of healthcare.”
Singletary cites a recent study published by the University of Maryland School of Medicine, which discovered that African American patients use emergency departments at higher rates than any other racial group. According to the study, African Americans use emergency departments 54% of the time for routine medical care. And in urban areas, African Americans use emergency rooms 59% of the time.
“At what point are these individuals expected to receive treatment for underlying health conditions?” Singletary said. “At what point will they receive primary or preventive care? What about health screening, tests for diabetes, high blood pressure and annual exams? There's no such thing as preventive or continuity of care [for these communities]. It's all rinse and repeat of emergency acute care. And this is tied directly to the wealth gap that is prevalent in the Black community.”
Tied to comorbidities are health habits and issues such as tobacco use, diet and stress, which further make these populations more vulnerable to COVID-19.
Additionally, many people in minority communities have low-wage jobs that are considered “essential,” meaning that they must go out and potentially be exposed daily to the virus.
Dr. Singletary recalls that during the height of the COVID-19 crisis this spring he went to a grocery store where three older Black gentlemen were working on the frontline. “You could tell from the looks on their faces that they had so much pride in their jobs. [But] they didn’t have masks on,” he said.
When he returned to the store three weeks later, only two of the men he had previously met were there. They all had been absent for a couple of weeks. “I asked them where their other guy was," says Singletary. “Finally, one of them said ‘Oh, you mean Jimmy, he died last week of the COVID-19.’”
One way to address racism and racial disparities in healthcare is to expand the healthcare workforce, and have healthcare providers that better understand, and are sensitive to, the health needs of different communities, Singletary says. Representation matters. Having healthcare providers who can build trust with underserved communities will impact, overall, the decision that constituents of those communities make about preventative and primary care. Another key point that needs to be addressed is access to quality healthcare for these communities, which is a heavy lift and will take many years to remedy.
Chamberlain University is dedicated to social justice commitments, which expand access of nursing and healthcare education to under-represented minority students. Chamberlain is the leading grantor of Bachelor of Science in Nursing degrees to minority students in the United States, effectively creating a healthcare workforce who have the unique opportunity to make a real impact on healthcare inequity.
Chamberlain students can also get involved with opportunities to impact diversity and inclusion in their own healthcare communities:
- Join the Student Government Association (SGA)
- Build a diversity and inclusion student group on your campus
Help us create a generation of nurses, social workers and other healthcare professionals who make an impact on eliminating healthcare inequity.
Related Stories
Diversity & Inclusion: How Do They Relate to Healthcare?
Why Black Women are More at Risk for Human Trafficking – and What Nurses Can Do to Help
By Kate Rice
More from Health Professions
Request More Information
To receive the Chamberlain University Program Guide, including associated career paths, please select a program of study.